Female Urinary Incontinence

- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
Description Female Urinary Incontinence
Urinary incontinence is the involuntary loss of urine, a condition that is more common in women than in men, among other reasons, because the female urethra is shorter.
Types of urinary incontinence
The types of incontinence, from a symptomatic point of view, can be classified in different ways:
- Stress urinary incontinence.
- Urgency urinary incontinence.
- Overflow urinary incontinence.
- Functional urinary incontinence.
- Mixed urinary incontinence.
When urinary incontinence is associated with an urgent and frequent urge to urinate both day and night, we speak of overactive bladder.
Each typology will be treated differently depending on whether the problem is related to the urinary sphincter and pelvic floor or bladder function. In some cases, patients also report vaginal bulge, this is genital prolapse, which is the descent of the pelvic organs due to weakness of the pelvic floor that supports them and may appear associated with urinary incontinence.
Risk factors of urinary incontinence
Common risk factors include pregnancy, childbirth, gynecological surgery, obesity, trauma or injury, among others. For its treatment, general measures such as weight control, adequacy of fluid intake, physical exercise and pelvic floor individualized to the patient are indicated in a first step.
To understand the functioning of the lower urinary system, we explain below the anatomical elements that interfere with the retention and expulsion of urine:
- Bladder: a hollow organ located in the lower abdomen that can hold up to two cups of urine for two to five hours. It is supported by ligaments attached to other organs and the bones of the pelvis. The walls of the bladder relax and dilate to collect urine, and contract to empty it through the urethra.
- Two sphincter muscles: circular muscles that help keep urine from leaking by closing tightly around the bladder opening.
- Bladder nerves: responsible for telling the person when it is time to urinate and empty the bladder.
- Urethra: the tube that carries urine from the bladder to the outside of the body. The brain sends signals to the bladder muscles to contract and expel the urine stored in the bladder. At the same time, the brain sends signals to the sphincter muscles to relax and allow urine to flow out of the bladder through the urethra. When all the signals occur in the correct order, the person urinates normally.
They ask us in the Consultation
I am able to hold my urine but I feel the urge to go to the bathroom quickly, is it incontinence?
Most patients with voiding urgency do not have urinary incontinence, but should consult a specialist.
If I drink less fluid, will I have fewer episodes of incontinence?
The amount of liquids ingested is directly related to the amount of urine produced. The appropriate amount is at least 1.5 liters, taking into account that all foods contain a variable volume of water. In the case of stress urinary incontinence, it may be useful to take the precaution of emptying the bladder when any activity involving physical exertion is planned.
What is the best treatment for urinary incontinence?
Treatment is individualized depending on the type of incontinence and severity. A study is required to see when the incontinence appears.
What exercises can I do to strengthen the pelvic floor?
In general, pelvic floor exercises performed with a specialist in pelvic floor physiotherapy are recommended.
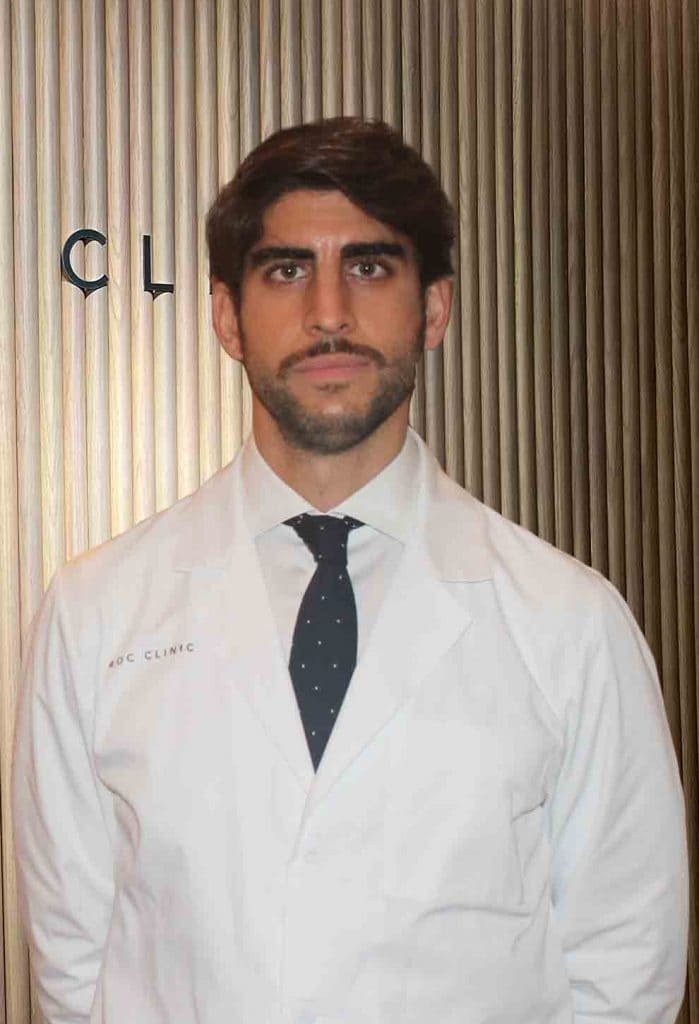
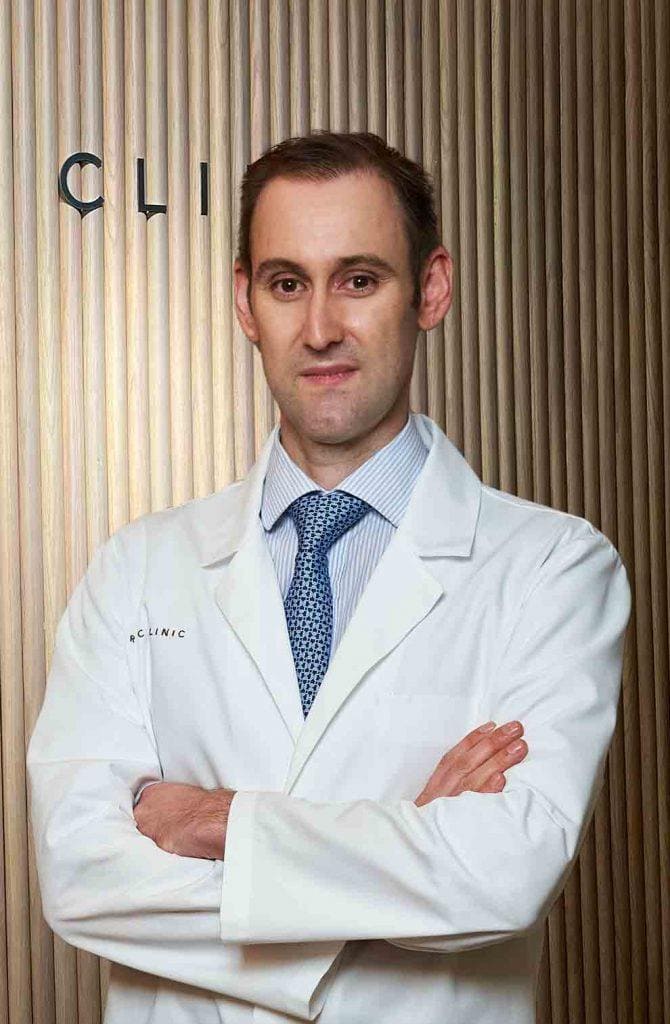
Team of the Female Urinary Incontinence Unit
Newsof ROC Clinic in Female Urinary Incontinence
Research
Diagnostic and therapeutic approach to nocturia in primary care.
Technology
Artificial urinary sphincter implant for severe cases of stress urinary incontinence.


 +34 912 627 104
+34 912 627 104 Contact
Contact