Symptoms and causes Female Urinary Incontinence
Involuntary urine loss can be classified differently depending on the symptoms it presents.
- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
Female Urinary Incontinence Symptoms
Urinary incontinence is the spontaneous loss of urine involuntarily, altering the patient's quality of life. These losses can appear in different circumstances such as physical exertion, coughing, sports, laughing, leaks at the end of urination, leaks triggered by the desire to urinate. There may also be urine leakage at the time of sexual intercourse.
Depending on the presenting symptoms, urinary incontinence can be classified as follows:
- Stress urinary incontinence. Urine leaks when pressure is exerted on the bladder during any type of effort such as walking, coughing, sneezing, laughing, playing sports, getting up from a chair or lifting something heavy. The reason is usually the anatomical alteration of the sphincter system and pelvic floor and may be associated with pelvic organ prolapse either of the bladder, uterus or rectum.
- Urge urinary incontinence. This is a sudden and intense need to urinate, followed by an involuntary loss of urine. You may have to urinate frequently (pollakiuria), even at night (nocturia). Urge urinary incontinence may be due to a minor condition, such as an infection, or a more serious disorder, such as a neurological disorder or diabetes. Overactive bladder is defined by urinary urgency, i.e., the sensation of the urge to urinate and the inability to delay urination. Women with urge incontinence usually have an overactive bladder. Approximately 50% of women leak urine, while the other 50% do not.
- Overflow incontinence. To give an example, it is as if the bladder fills up like a reservoir and the water overflows by jumping over the dam. Patients with this type of incontinence usually have a bladder problem. The bladder does not have the strength to contract, so when it is full, urine leaks out. This type of incontinence appears in patients with an obstruction in the urinary tract, or in patients who have a neurological disorder due to a heart attack, multiple sclerosis, etc.
- Functional incontinence. This type of incontinence occurs when a physical or mental disability prevents you from getting to the bathroom in time. For example, if you have severe arthritis, you may not be able to unbutton your pants fast enough.
- Mixed urinary incontinence. When there is more than one type of urinary incontinence at a time. Most often it is a combination of stress and urge incontinence.
Causes of Female Urinary Incontinence
Urinary incontinence can be caused by certain daily habits, underlying diseases or physical problems. A thorough evaluation by your health care provider can help determine what is causing the incontinence.
- Physical problems or underlying changes: Common risk factors include pregnancy, childbirth, gynecological surgery, obesity, trauma or injury, among others. For its treatment, general measures such as weight control, adequacy of fluid intake, physical exercise and pelvic floor individualized to the patient are indicated in a first step.
- Pregnancy: hormonal changes and the weight of the fetus can lead to stress incontinence. Pregnancy changes the physiognomy and anatomy of the pelvic floor causing urine to leak. If the woman suffering from stress incontinence has a weak pelvic floor or a pelvic floor disorder, this can lead to an increased risk of postpartum incontinence.
- Vaginal delivery: can weaken the muscles that help control the bladder and damage nerves and tissue causing the pelvic floor to drop (prolapse). Prolapse can cause the bladder, uterus, rectum, or small bowel to fall.
- Age: Aging of the bladder muscle can decrease the ability to store urine. In addition, involuntary bladder contractions become more frequent as you age.
- Menopause: After menopause, women produce less estrogen, a hormone that helps preserve the membrane lining the bladder and urethra. Deterioration of these tissues can aggravate incontinence.
- Neurological disorders: Multiple sclerosis, Parkinson's disease, stroke, brain tumor or spinal cord injury can damage the nerve signals involved in bladder control and cause urinary incontinence.
- Beverages and medications: Also, some beverages, foods and medications can act as diuretics that stimulate the bladder and increase urine volume. Some of these substances are: alcohol, coffee, soft drinks, sweeteners, chocolate, hot peppers, spices, sugar, citrus fruits, blood pressure and heart medications, sedatives and muscle relaxants, and high doses of vitamin C.
- Urinary tract infections: On the other hand, urinary tract infections can irritate the bladder and cause a strong urge to urinate and sometimes incontinence.
- Constipation: Constipation also worsens urinary incontinence, as the rectum is located close to the bladder and shares many nerves.
- Overweight: Excess weight increases pressure on the bladder and surrounding muscles, which weakens them and allows you to leak urine when you cough or sneeze.
- Smoking: Smoking may increase the risk of urinary incontinence.
- Family history: If a close relative has urinary incontinence, the risk of developing the condition is higher.
Complications
If urinary symptoms in women are not adequately treated, they can lead to their worsening and the progression of the mechanisms involved, such as pelvic floor weakness, making treatment more difficult.
Other complications that may occur are:
- Skin problems. Rashes, skin infections and sores may occur as a result of constant wetness.
- Urinary tract infections. Incontinence increases the risk of recurrent urinary tract infections.
- Impact on personal life: may affect social, work and personal relationships.
Prevention
Although urinary incontinence cannot always be prevented, you can reduce your risk by living a healthy lifestyle with physical exercise, avoiding foods that irritate the bladder, eating more fiber and quitting smoking.
They ask us in the Consultation
If I drink less fluid, will I have fewer episodes of incontinence?
The amount of liquids ingested is directly related to the amount of urine produced. The appropriate amount is at least 1.5 liters, taking into account that all foods contain a variable volume of water. In the case of stress urinary incontinence, it may be useful to take the precaution of emptying the bladder when any activity involving physical exertion is planned.
What is the best treatment for urinary incontinence?
Treatment is individualized depending on the type of incontinence and severity. A study is required to see when the incontinence appears.
What exercises can I do to strengthen the pelvic floor?
In general, pelvic floor exercises performed with a specialist in pelvic floor physiotherapy are recommended.
How to avoid urinary incontinence during pregnancy?
In general, an active lifestyle, avoidance of excess weight and assessment by a specialist in pelvic floor physiotherapy are recommended.
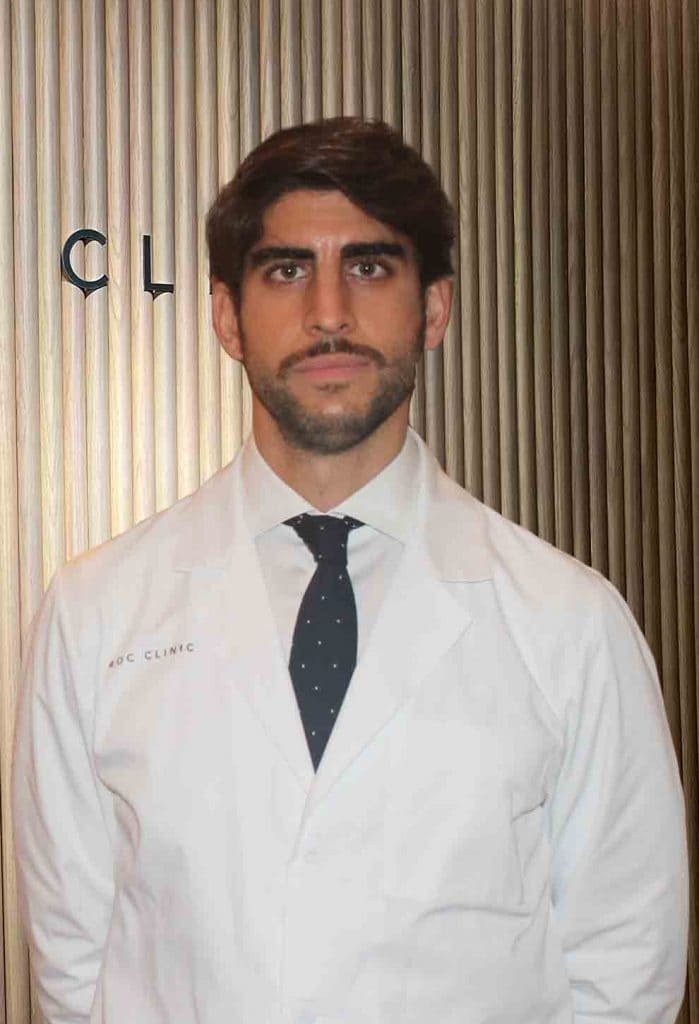
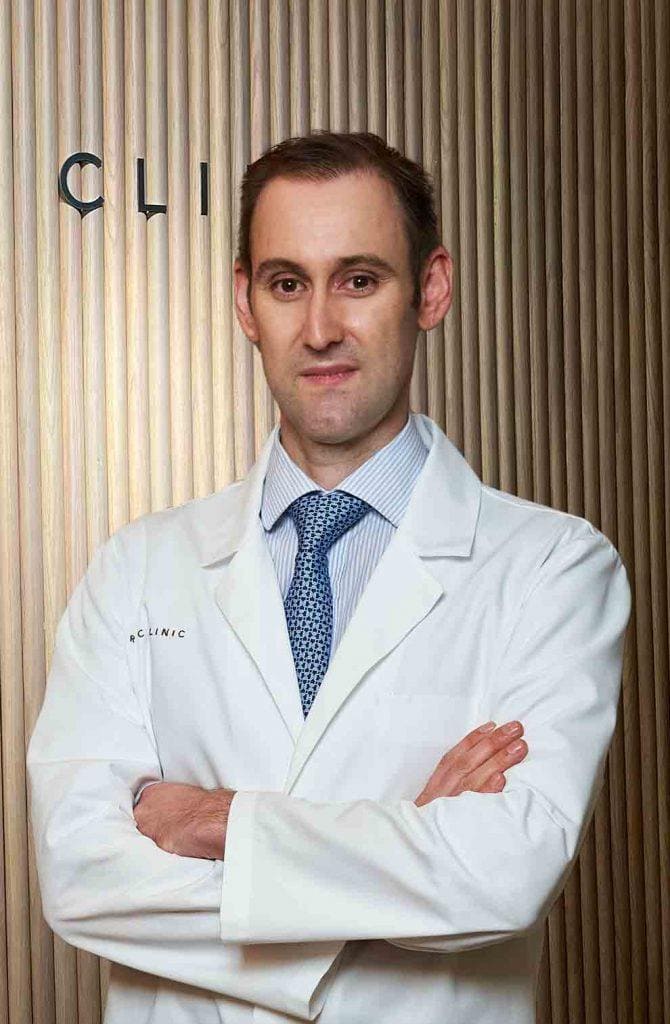
Team of the Female Urinary Incontinence Unit
Newsof ROC Clinic in Female Urinary Incontinence
Research
Diagnostic and therapeutic approach to nocturia in primary care.
Technology
Artificial urinary sphincter implant for severe cases of stress urinary incontinence.


 +34 912 627 104
+34 912 627 104 Contact
Contact