Bladder cancer


- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
What is bladder cancer?
Bladder cancer is a disease originating in the layer that lines the inside of the bladder, a layer that is also found in the ureters and reaches the kidneys. Therefore, it is also necessary to periodically check the upper urinary tract - from the bladder to the kidneys - for relapses or the appearance of new tumors in this area.
Fortunately, most of these tumors (around 75% of cases) are diagnosed at a non-muscle-invasive stage, i.e. when the root has not yet reached the bladder muscle, called the detrusor muscle. However, one of the main problems of this cancer is its high rate of recurrence and progression. In other words, the tumor tends to recur and, in some of these relapses, it can invade the muscle.
For this reason, it is important to carry out periodic check-ups to rule out its reappearance, even after having undergone intravesical lavage treatments with chemotherapy instillations or BCG (bacillus Calmette-Guérin) immunotherapy through a catheter.
About the bladder
The urinary bladder is a hollow muscular organ responsible for storing urine for later emptying. Urine is produced in the kidneys and reaches the bladder through ducts called ureters. Once stored in the bladder, the bladder muscle or detrusor muscle - a layer of muscle that forms part of the wall of the urinary bladder - contracts and causes the urine to be expelled through the urethra.
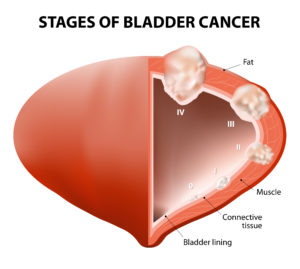
Inside, the bladder has a thin layer that covers it on the inside: the urothelium. Immediately after the urothelium is the lamina propria, a tissue that is surrounded by the bladder muscle, covered in turn by fat and by a membrane on its surface called the peritoneum.
How does bladder cancer form?
Cancer is characterized by the development of abnormal cells that divide, grow and spread uncontrollably. Normal cells divide and die during a programmed period of time. However, cancer cells lose the ability to die and divide uncontrollably. This multiplication of cells eventually forms masses called tumors.
In bladder cancer, the transformation from normal to cancerous cells usually originates in the urothelium. Fortunately, in most cases it is diagnosed before the roots of the tumor penetrate the urothelium and the next layer, the lamina propria, and therefore have not invaded the muscularis layer. These are the so-called non-muscle-infiltrating bladder tumors. They are malignant tumors, but their location gives them the characteristic of being non-invasive, that is, they have not spread to the muscular layer.
Tumors that invade the muscular layer, called muscle-infiltrating tumors, represent a higher risk and have fewer and more aggressive therapeutic options.
A cancer is said to be recurrent when it reappears after treatment. The recurrence or recurrence can be local, located where it started or near this area, or at a distance in the form of metastasis, spread to other organs or bones.
They ask us in the Consultation
Does a urine culture detect cancer?
No, a urine culture does not detect cancer, as its purpose is to identify urinary tract infections through the presence of bacteria. However, other urine tests, such as a urinalysis or urine cytology, may suggest the presence of cancer by detecting blood or abnormal cells in the urine. If there is suspicion of cancer in the urinary system, additional studies such as biomarker tests, ultrasound, CT scans or biopsies are required to confirm the diagnosis. If you detect blood in the urine with no apparent cause, it is essential to see a physician for further evaluation.
What are the most common symptoms of bladder cancer?
Bleeding in the urine, stinging when urinating or the sensation of incomplete voiding.
When should bleeding in the urine be studied?
When the bleeding is visible to the naked eye, it should always be studied. When it is microscopic, i.e., it is not visible to the naked eye, when it must be studied whenever it is significant (more than 3 red blood cells per field) especially in patients with risk factors: over 40 years of age or smokers or exposed to certain dye or paint substances.
What is the prognosis of bladder cancer?
In general it is good. These tumors are usually diagnosed before they infiltrate the muscle, allowing the bladder to be preserved. The problem lies in the fact that it is a chronic disease that has recurrence and relapses over time. It requires many check-ups and treatments and the patient must adhere to them without skipping check-ups, which can lead to metastasis.
Team of the Bladder Cancer unit
Newsof ROC Clinic in Bladder Cancer
Research
Ureteral metastasis of a prostatic adenocarcinoma
Technology
Radical cystectomy by Da Vinci robotic surgery for maximum precision and minimum aggressiveness.
Training
Training on the controversies in non-muscle invasive bladder and upper urinary tract tumors by Dr. Felix Guerrero Ramos at the AEU.


 +34 912 627 104
+34 912 627 104 Contact
Contact