Overactive Bladder
- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
What is overactive bladder?
Overactive bladder is defined by frequent (pollakiuria) and urgent urination. It occurs when the bladder muscles begin to contract involuntarily even though the volume of urine stored in the bladder is low.
People with overactive bladder may go to the toilet more than 12 times a day or every half hour and may also need to get up frequently at night to go to the bathroom (nocturia). This greatly affects the sufferer's quality of life, as it can limit their social and work life.
This condition affects about 25% of women and 20% of men. Even so, there are many undiagnosed cases because sufferers do not give it importance, consider it normal or are embarrassed to see a specialist.
To combat the symptoms, the sufferer can start by trying some habit changes such as diet modification, timed voiding strategies or bladder containment techniques using the pelvic floor muscles. Also, leading a healthy lifestyle can help reduce the risk of overactive bladder:
- Maintain a healthy weight.
- Daily physical activity and exercise.
- Reduce caffeine and alcohol consumption.
- Smoking cessation.
- Control chronic conditions, such as diabetes, which can enhance overactive bladder symptoms.
- Strengthen the pelvic floor with exercises such as Kegel exercises. Some of these exercises involve tensing or contracting the muscles, holding the contraction for two seconds and then relaxing the muscles for three seconds. Then gradually increase the time until you hold the contraction for five seconds and then for ten seconds. Perform three sets of ten repetitions per day.
If these guidelines do not help enough, a physician can evaluate if there is a specific cause and prescribe appropriate treatment.
They ask us in the Consultation
Is overactive bladder incontinence related to age?
Overactive bladder, unlike stress urinary incontinence, does not have such a marked component with age, so it also appears in younger people.
Are Kegel pelvic floor exercises effective for overactive bladder?
Overactive bladder is related to involuntary bladder muscle contractions, so rehabilitation exercises are focused on the bladder.
I have been told I have an overactive bladder, do I have to have prostate surgery?
Men also have symptoms of overactive bladder and specific treatment should be considered.
How is overactive bladder treated?
In addition to hygienic-dietary measures, there are specific oral and patch drugs for the treatment of overactive bladder. The use of botulinum toxin is also useful to manage overactive bladder.
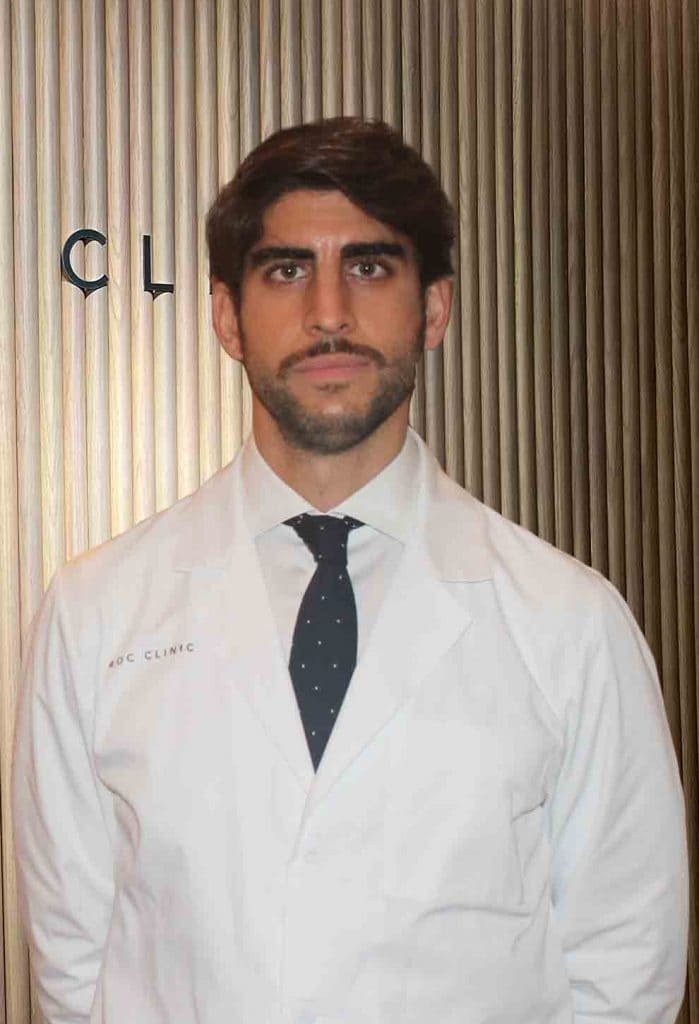
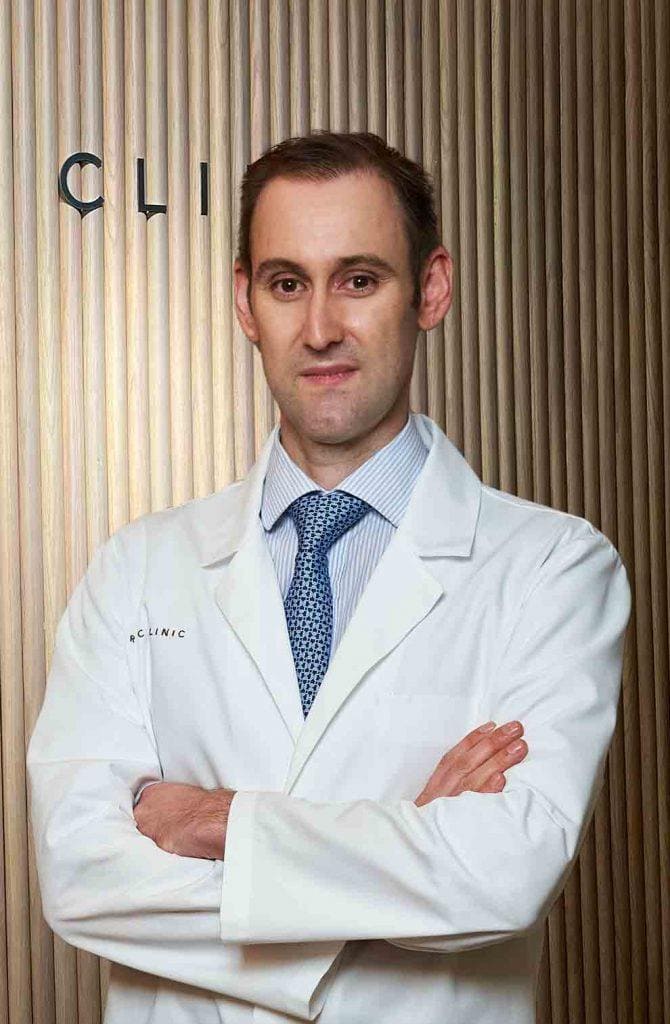
Team of the Overactive Bladder Unit
Newsof ROC Clinic on Overactive Bladder
Research
Combined laparoscopic surgery for the treatment of pelvic organ prolapse and recurrent urinary incontinence


 +34 912 627 104
+34 912 627 104 Contact
Contact