Diagnosis Overactive Bladder
Any other disease must be ruled out before an overactive bladder can be correctly diagnosed.
Overactive bladder affects about 25% of women and 20% of men. Even so, there are many undiagnosed cases because patients do not give it importance, consider it to be normal or are embarrassed to see a specialist.
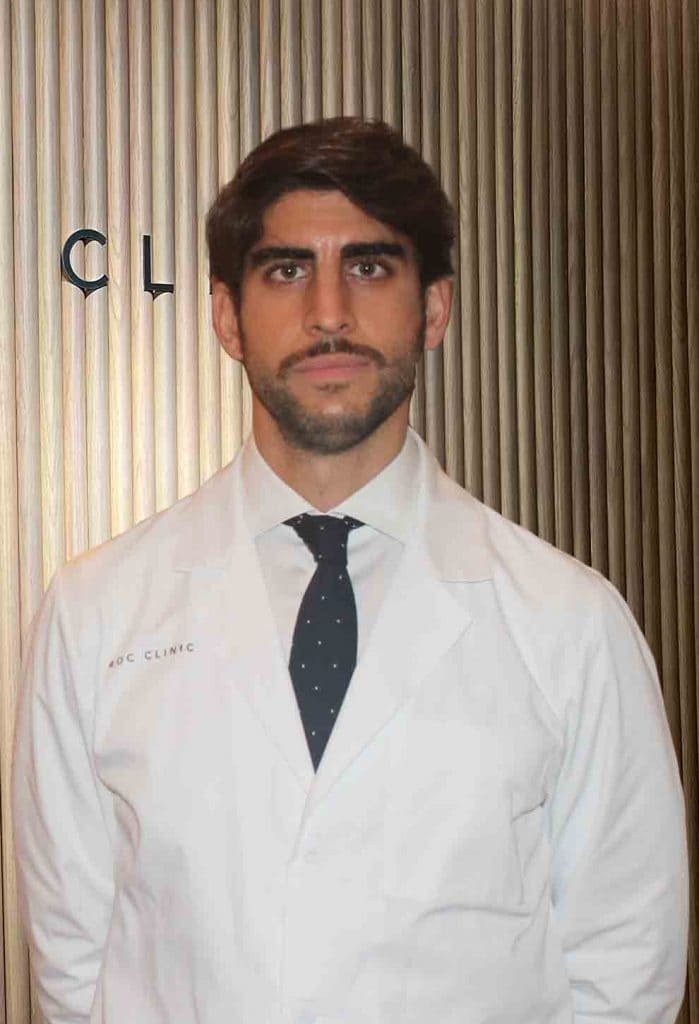
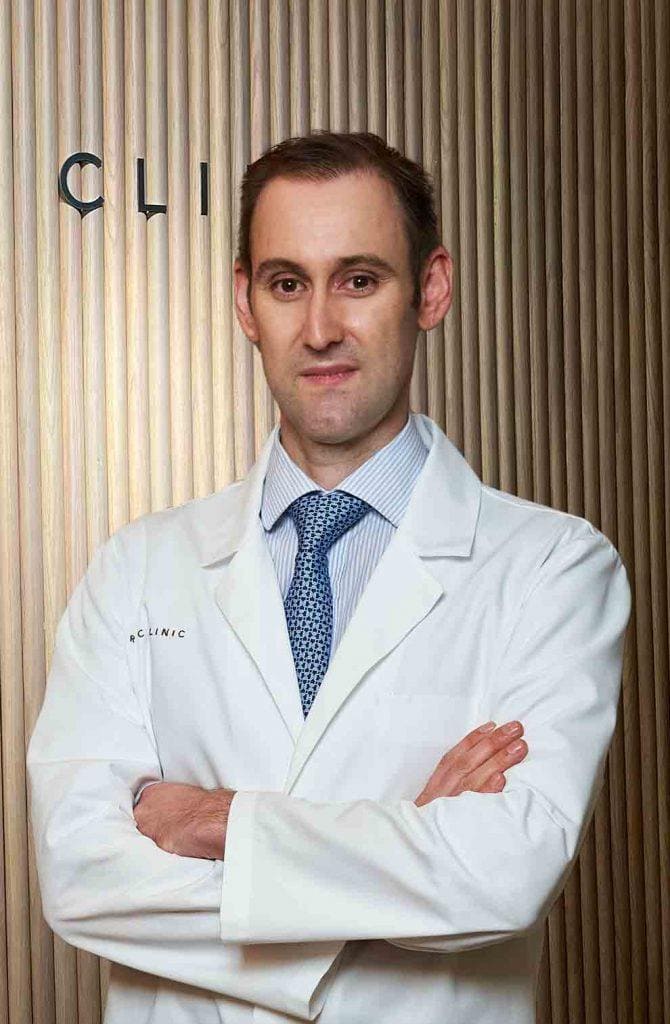
- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
Diagnosis of overactive bladder
Overactive bladder is characterized by the presence of urinary urgency - with or without urinary incontinence - associated with increased daytime and nighttime frequency of urination. For its diagnosis, the physician must document all the symptoms and signs presented by the patient and exclude the existence of other pathologies that could cause the symptoms.
Initial evaluation of patients with overactive bladder should include:
Medical history:
It is essential in the initial evaluation and should collect the type, time and severity of symptoms, as well as the presence or absence of urinary incontinence. In addition, it should allow differentiation of urgency urinary incontinence from stress urinary incontinence and mixed urinary incontinence.
It is important to reflect the symptoms clearly and avoid ambiguous terms so that there can be no confusion. For example, you should collect daytime voiding frequency, times between micturitions, nighttime voiding frequency, number of times you get up to urinate at night.
Also, the medical history should include any pathology the patient may have, as well as the pharmacological treatments he/she is receiving to check if they can have any impact on or cause overactive bladder symptoms.
On the other hand, possible symptoms and/or history suggesting the need for referral for further study should be detected. If there is the presence of hypogastric or perineal pain, before, during or after urination, the patient should not be classified as having overactive bladder syndrome.
Physical examination:
It includes abdominal examination to detect increased bladder volume or the presence of other abdominal masses.
In men, a rectal examination should be performed and in women the estrogenic status and the possible presence of prolapse (descent of the pelvic organs due to weakening of the pelvic floor) should be evaluated.
Urinalysis:
It is performed to rule out the presence of urinary tract infection or hematuria. Urine sediment must be performed to be sure that there is no organic alteration in the bladder causing the symptoms: urinary tract infection, hematuria, leukocyturia, suspected bladder lithiasis.
Voiding diary:
Voiding diaries are a reliable tool for measuring voiding volume, urinary frequency and episodes of voiding urgency and incontinence. It also serves to measure the evolution and results after treatment.
Questionnaires:
Based on scoring scales and validated symptom questionnaires in Spanish that have proven to be useful in measuring changes in patients' condition. This tool allows to measure the severity of symptoms, as well as to screen or classify urinary incontinence if present and help determine if a change in treatment is needed.
On the other hand, the impact of overactive bladder symptoms on quality of life is an important aspect in its management.
Other tests:
- Determination of postvoid residual: it is not necessary in patients without complications, but in those who have symptoms of incomplete bladder emptying, complicated urinary incontinence or who receive treatments that could cause or worsen voiding symptoms.
- Flowmetry: due to the high incidence of prostate enlargement in men over 50 years of age, which may affect bladder emptying, it is advisable to perform flowmetry.
- Urodynamics: to be performed in case of incontinence, when there is no response to initial treatment, when there has been previous surgery in the lower urinary tract or when there is a neurogenic disease.
- Cystoscopy and imaging: to be performed in case of pathological sediment and suspicion of organic bladder involvement.
They ask us in the Consultation
Is an overactive bladder operated on?
In case of pelvic floor weakness and stress incontinence, surgery is performed for the treatment of stress urinary incontinence. However, in case of overactive bladder there is no clear surgical treatment.
Is urodynamic study useful in cases of overactive bladder?
Patients with overactive bladder show in the urodynamic study detrusor bladder muscle contractions during filling, which allows the diagnosis of overactive detrusor. In addition, the urodynamic study provides information on bladder capacity, the elastic capacities of the bladder, how bladder emptying works and the presence of stress urinary incontinence, among others.
Is overactive bladder incontinence related to age?
Overactive bladder, unlike stress urinary incontinence, does not have such a marked component with age, so it also appears in younger people.
Are Kegel pelvic floor exercises effective for overactive bladder?
Overactive bladder is related to involuntary bladder muscle contractions, so rehabilitation exercises are focused on the bladder.
Team of the Overactive Bladder Unit
Newsof ROC Clinic on Overactive Bladder
Research
Combined laparoscopic surgery for the treatment of pelvic organ prolapse and recurrent urinary incontinence


 +34 912 627 104
+34 912 627 104 Contact
Contact