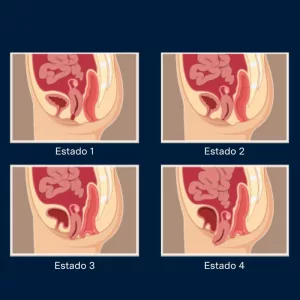
Pelvic organ prolapse is the descent of the pelvic organs (bladder, uterus, rectum or bowel) through the vagina that occurs as a result of the weakness of the pelvic floor support elements (ligaments and muscles).
This weakness can have multiple causes: childbirth, overweight, predisposition of the patient, pelvic surgery, trauma... It is estimated that up to 12% of women will require surgical treatment for prolapse during their lifetime.
The symptoms associated with pelvic organ prolapse are very variable and range from the absence of symptoms to voiding problems (incontinence, difficulty urinating, imperious urination...), to problems in the sexual sphere or constipation.
Diagnosis of prolapseThe diagnosis of pelvic organ prolapse is eminently clinical. The urologist will establish the diagnosis of prolapse and its severity by means of a detailed clinical history and correct physical examination.
The diagnosis will be completed with individualized tests in each case, which will provide more information. These tests can be: urological and pelvic floor ultrasound, questionnaires, bladder function studies (flowmetry and urodynamic study), urine culture, etc.
Treatment of prolapse
The treatment of pelvic organ prolapse will be individualized in each case according to the severity, symptoms and wishes of the patient. It can be classified into two types:
Conservative treatment of prolapse
- Lifestyle changes. Weight loss can improve pelvic organ prolapse (POP) in overweight women.
- Pelvic floor rehabilitation. This is the most desirable option in patients with mild, mildly symptomatic prolapse. However, it has not been shown to reduce the severity of prolapse.
- Pessary: this is a device that is placed inside the vagina. It is an option in patients with high surgical risk or who do not wish to undergo surgery. It requires replacement and periodic monitoring.
Surgical treatment of prolapse
Prolapse repair surgery aims to reposition the pelvic organs in their original position. The results are highly variable depending on the surgical technique used for pelvic organ prolapse repair. The technique is decided based on the characteristics of the prolapse and the patient's expectations:
- Vaginal surgery without mesh. It consists of prolapse repair by techniques that use the patient's own tissues. It is especially indicated in patients with high surgical risk or mild prolapse.
- Robot-assisted colposacropexy. This is a minimally invasive technique that allows repair of the pelvic floor by implanting an intra-abdominal mesh. The advantages of robotic surgery over conventional surgery are a more precise and safer repair, with an exceptionally clear three-dimensional view for the surgeon of the patient's anatomy, a faster recovery and a lower rate of both intraoperative and postoperative complications. The risk of bleeding is reduced, postoperative discomfort is reduced and scarring is minimal.
Robotic colposacropexy is performed under general anesthesia. After the procedure is performed, the average hospital stay is 24-48 hours. You can usually go home without a bladder catheter.
Postoperative
Surgical wounds should be washed with soap and water and kept dry. Your surgeon will tell you when to check them for staple removal. In the days or weeks following surgery, you may experience changes in your bowel habits. For this reason, your doctor will recommend a diet rich in fiber, good water intake and even use a mild laxative if necessary.
It is essential for the patient to keep relative rest (avoid physical exercise, exertion, sexual relations...) for 4-6 weeks to achieve adequate healing and optimal results.
Results and quality of life
The main objective of pelvic floor repair is to improve the quality of life of patients, since prolapse has repercussions not only from the point of view of the symptoms it produces, but also affects the social and occupational sphere. Minimally invasive surgery, such as robotic colposacropexy, has proven to be a safe surgery with excellent medium and long-term results. In experienced hands such as ours, the success rate is over 90% and most of our patients require a 24-48 hour hospital stay, with a quick return to normal life.




 +34 912 627 104
+34 912 627 104 Contact
Contact