Testicular Cancer
- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
What is testicular cancer?
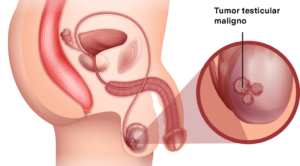
Testicular cancer occurs when cells begin to grow uncontrollably in the testicles. To understand this cancer, it is helpful to know the normal structure of the testicles and their function.
The testicles are two organs of the male reproductive system that are located inside a sac of skin called the scrotum that hangs below the base of the penis. Their two main functions are:
- Produce male hormones (androgens), such as testosterone.
- Produce sperm, which are the male cells that fertilize the female sex cell (egg), and thus start a pregnancy.
Sperm cells are produced in long, thin tubes located inside the testicles called seminiferous tubules. These cells are stored and mature in the epididymis, a small coiled tube located behind each testicle.
During ejaculation, sperm cells move from the epididymis through the vas deferens to the seminal vesicles, where they mix with fluids produced by the seminal vesicles, the prostate gland and other glands to form semen. Finally, this fluid enters the urethra (the tube inside the penis through which urine and semen pass) to exit to the outside.
Testicular cancer usually manifests as a painless scrotal mass of recent onset. In some cases, the testicular tumor may debut metastatic, by local, retroperitoneal progression or distant metastasis. In that case, the symptoms will depend on the location of the tumor.
There are several types of testicular tumor. Their prognosis and nature is diverse, and depending on their histological type they will respond better to certain treatments.
The best initial diagnostic test is physical examination and scrotal ultrasound. Testicular ultrasound is the gold standard system and provides a lot of information about the existence or not of a tumor, the local affectation it produces and the invasion of neighboring organs.
In case of suspicion of testicular tumor by examination or ultrasound, the next step is to perform tumor markers, which have diagnostic and prognostic power. They are usually performed before surgery (Beta-HCG, alpha-fetoprotein, LDH) and also during the follow-up of the disease. In addition, it is important to request a thoracoabdominal CT scan to detect the presence of lymph nodes or metastases, which testicular cancer produces early.
Treatment is usually performed by surgery. The first step is total or partial removal of the testicle. The former is usually chosen, although partial surgery can be safely performed as long as the tumor is not larger than one third of the testicle.
Orchiectomy is performed through an inguinal incision. The cord structures are checked early to prevent the emission of tumor cells, and the turmoral mass is removed. The placement of a penile prosthesis, for cosmetic purposes, is an option, depending on the preference of each man.
The post-operative period is usually short and benign. It is usual that the patient can be discharged even on the same day of surgery, being summoned for consultation in approximately 15 days to communicate the result of the biopsy.
In cases of high-risk testicular cancer or with metastases or adenopathies at the time of diagnosis, chemotherapy is generally applied very effectively. Even in advanced cases, it is a curable disease thanks to the combination of chemotherapy and, sometimes, also radiotherapy and surgery.
However, the testicular tumor can recur quickly, so the initial controls must be very intense and exhaustive.
Side effects of treatment
As a result of surgery and chemotherapy for the treatment of testicular cancer, men may experience various side effects:
- Alteration of self-image, which can be counteracted, in part, by the placement of the teste prosthesis.
- Decreased testosterone. The existence of a single testicle increases the risk of presenting a decrease in testosterone with the consequences that this entails: erectile dysfunction, decreased sexual desire, obesity, loss of muscle mass, peripheral insulin resistance, osteoporosis, increased cardiovascular or prostate risk.
- Impairment of fertility. Many of the treatments can alter fertility. In this sense, sperm cryopreservation can be used before the start of systemic treatments (chemotherapy and radiotherapy) to try to have biological material that has not been affected by the toxicities of these treatments.
They ask us in the Consultation
When is the use of robotic surgery recommended?
Robotic surgery is recommended in a variety of situations where its advantages can significantly improve patient outcomes compared to traditional open or laparoscopic surgery. It is considered especially beneficial in complex procedures where high precision and surgical dexterity are required in confined spaces, in patients with comorbidities and/or when urinary or erectile function is sought to be preserved.
Can testicular tumor be cured?
Yes, the vast majority of testicular cancers are curable. The earlier we make the diagnosis, the better the chances of cure with minimal treatment.
What is the treatment for testicular cancer?
First we perform surgery to determine the type of tumor and its local extension. Then, depending on various factors, other treatments may be necessary.
Does it affect my fertility if I have a testicle removed?
This is a possibility, although it is not always the case. Many young men preserve sperm prior to surgery in order to have healthy sperm available when they consider having offspring.
Team of the Testicular Cancer Unit
Newsof ROC Clinic in Testicular Cancer
Research
Metastatic testicular cancer presenting with hematuria and flank pain


 +34 912 627 104
+34 912 627 104 Contact
Contact