Diagnosis Testicular Cancer
Testicular cancer is a fast-growing disease. Early diagnosis is essential to prevent progression of the disease.
The best initial diagnostic test is physical examination and scrotal ultrasound. Testicular ultrasound is the gold standard system and provides a lot of information about the existence or not of a tumor, the local affectation it produces and the invasion of neighboring organs.
- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
Diagnosis of testicular cancer
For the diagnosis of testicular cancer, in addition to an adequate physical examination, the following diagnostic tests are performed:
- Blood tests with testicular tumor markers, which are elevated in 51% of cases. They also serve to establish prognosis and are useful in follow-up. They are B-HCG, alpha-fetoprotein and LDH. They are always taken before and after testicular removal surgery.
- Imaging test. In any man with a new onset scrotal mass or pain, especially in those under 40 years of age, it is reasonable to request a scrotal ultrasound. Scrotal ultrasound is the gold standard test for the diagnosis of scrotal pathology, and also in testicular cancer.
Doppler ultrasound makes it possible to study the structure of the testicles and their blood vessels, and to determine if there is any mass, as well as its extension. The use of testicular ultrasound can:
- Determine whether a mass is intra- or extra-testicular.
- Determine the volume and anatomical location of the lesion.
- Characterize the contralateral testicle to exclude other lesions and identify risk factors for neoplasia.
Testicular ultrasound is also recommended for all men with retroperitoneal or visceral masses and/or no elevation of testicular tumor markers in the absence of a palpable testicular mass. When in doubt, scrotal magnetic resonance imaging (MRI) may be performed.
- Thoracic-abdominal-pelvic CT. In all cases in which testicular neoplasia has been diagnosed, it is necessary to perform a CT scan of the thorax and abdomen to rule out the presence of distant metastases.In selected cases brain CT may be performed if there is suspicion of brain metastases.
- PET. It is not used as an initial diagnostic test, but to evaluate the presence of retroperitoneal tumor despite chemotherapy treatment.
- In young patients who wish to have offspring in the future, a fertility study by seminogram and hormonal study (testosterone, LH and FSH) and the possibility of cryopreserving semen should be offered.
Types of testicular tumors
It is very important to classify the type of tumor after surgery, as they have very important implications for treatment and diagnosis. There are two main subgroups of testicular tumors.
Germ cell tumors:
They are the most frequent subtype (90-95% of cases) and are in turn classified into:
- Seminomas (35% of the total). They tend to grow and spread more slowly than non-seminomas.
- Non-seminomas (25% of the total): intratubular germ cell neoplasm, embryonal carcinoma, teratoma, teratocarcinoma, choriocarcinoma or yolk sac tumor).
- Mixed tumors (up to 40% of cases)
Stromal cell tumors:
- Leydig cell tumor: It is the most frequent stromal tumor. It appears in the first decade of life or between the third and sixth. Only 10% are malignant.It is diagnosed by the presence of painless testicular mass, gynecomastia and hormonal alterations. Treatment is surgical (in some cases conservative surgery can be performed) and metastatic cases show little response to chemotherapy or radiotherapy.
- Sertoli cell tumor: Appears around the age of 45 years. 20% are malignant, but have low metastatic capacity. It appears as a testicular mass and rarely presents gynecomastia or hormonal alterations. Treatment is surgical, with the possibility of conservative surgery in some cases.
They ask us in the Consultation
When is the use of robotic surgery recommended?
Robotic surgery is recommended in a variety of situations where its advantages can significantly improve patient outcomes compared to traditional open or laparoscopic surgery. It is considered especially beneficial in complex procedures where high precision and surgical dexterity are required in confined spaces, in patients with comorbidities and/or when urinary or erectile function is sought to be preserved.
Can testicular tumor be cured?
Yes, the vast majority of testicular cancers are curable. The earlier we make the diagnosis, the better the chances of cure with minimal treatment.
What is the treatment for testicular cancer?
First we perform surgery to determine the type of tumor and its local extension. Then, depending on various factors, other treatments may be necessary.
Does it affect my fertility if I have a testicle removed?
This is a possibility, although it is not always the case. Many young men preserve sperm prior to surgery in order to have healthy sperm available when they consider having offspring.
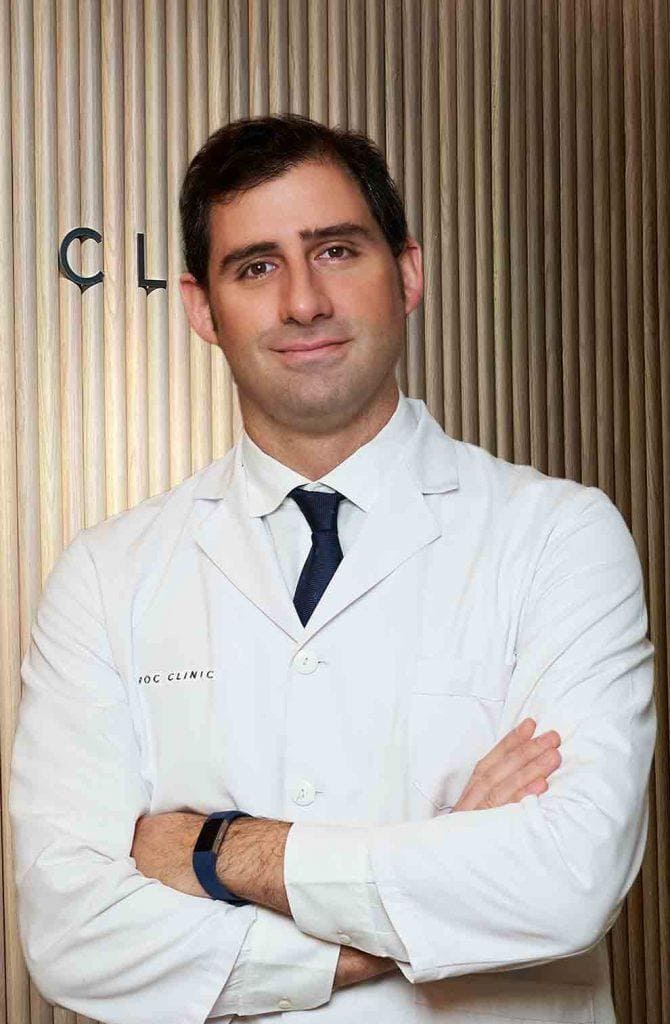
Team of the Testicular Cancer Unit
Newsof ROC Clinic in Testicular Cancer
Research
Metastatic testicular cancer presenting with hematuria and flank pain


 +34 912 627 104
+34 912 627 104 Contact
Contact