Treatment Female Urinary Incontinence
- Super-specialized urologists
- Personalized treatment
- Minimally invasive approach
- More than 16,000 patients successfully treated
Treatments and Technology
They ask us in the Consultation
If I drink less fluid, will I have fewer episodes of incontinence?
The amount of liquids ingested is directly related to the amount of urine produced. The appropriate amount is at least 1.5 liters, taking into account that all foods contain a variable volume of water. In the case of stress urinary incontinence, it may be useful to take the precaution of emptying the bladder when any activity involving physical exertion is planned.
What is the best treatment for urinary incontinence?
Treatment is individualized depending on the type of incontinence and severity. A study is required to see when the incontinence appears.
What exercises can I do to strengthen the pelvic floor?
In general, pelvic floor exercises performed with a specialist in pelvic floor physiotherapy are recommended.
How to avoid urinary incontinence during pregnancy?
In general, an active lifestyle, avoidance of excess weight and assessment by a specialist in pelvic floor physiotherapy are recommended.
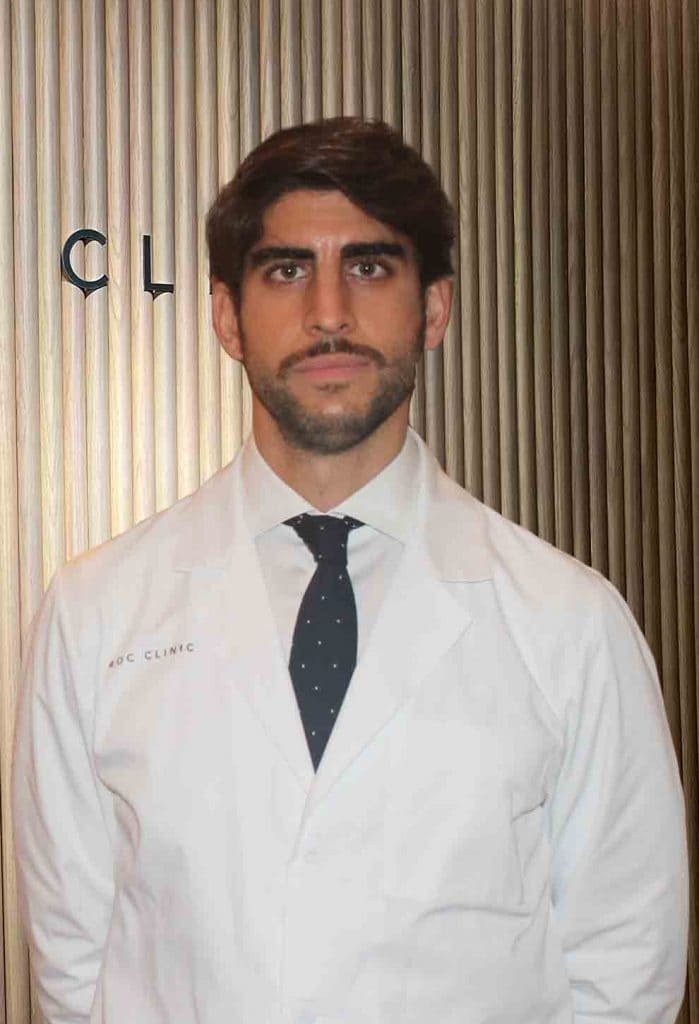
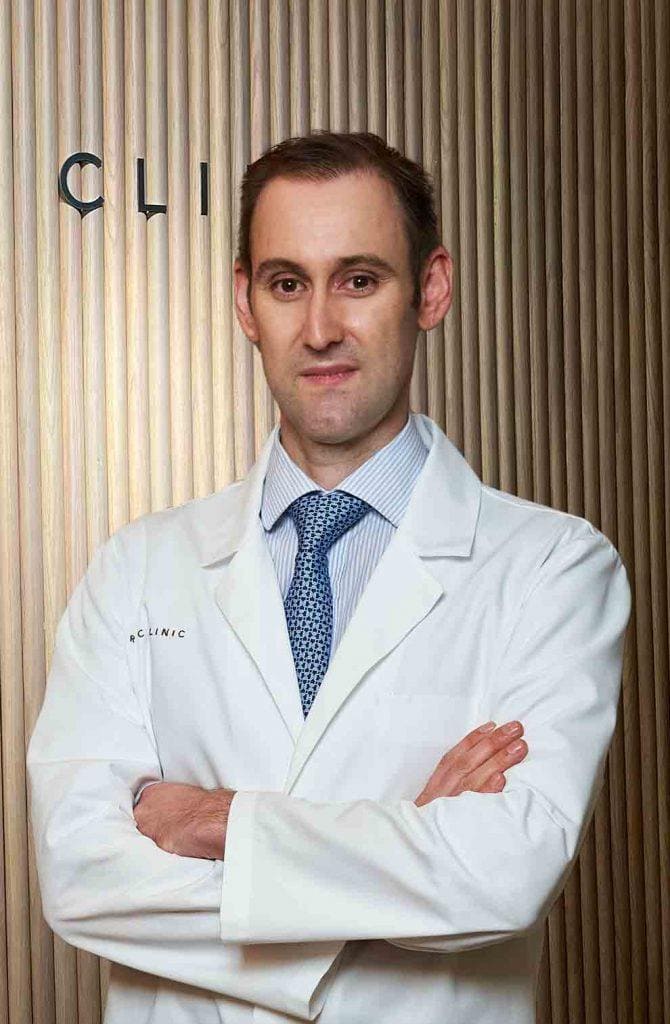
Team of the Female Urinary Incontinence Unit
Newsof ROC Clinic in Female Urinary Incontinence
Research
Diagnostic and therapeutic approach to nocturia in primary care.
Technology
Artificial urinary sphincter implant for severe cases of stress urinary incontinence.


 +34 912 627 104
+34 912 627 104 Contact
Contact